Full-arch restorations are a life-changing solution for those with extensive tooth loss, restoring function and facial aesthetics. For patients who have faced long-term dental issues, these solutions offer improved chewing, speaking, and a regained sense of confidence. However, while the initial results are impressive, the longevity of these restorations depends on various factors, highlighting the importance of understanding what influences their durability for lasting outcomes.
For those considering advanced treatment options like All-On-4 full mouth implants in Tulsa, OK, being aware of the variables that shape successful outcomes and sustained results is vital. Long-lasting results come from careful planning, patient commitment, clinical skill, and ongoing maintenance, not a single decision or product. Every step diagnosis, material choice, surgery, and aftercare—interdependently affects the success of full-arch restoration. This article examines key factors that contribute to durability, patient satisfaction, and functionality, enabling patients to make informed decisions about their oral health.
Patient Health Considerations
The success of full-arch restorations depends on the patient’s overall health. Conditions like uncontrolled diabetes, osteoporosis, cardiovascular or immune disorders hinder healing and raise implant failure risks. Unregulated blood sugar impairs healing and increases the risk of infection. Osteoporosis affects implant stability. Lifestyle factors like smoking reduce blood flow, slow healing, and increase peri-implantitis risk, risking restoration loss. Dentists often require smoking cessation and health management before surgery. Pre-treatment evaluation, specialist care, and patient involvement are vital for reducing risks and ensuring long-term success.
Material Selection and Prosthetic Design
Modern advances like high-performance polymers, nano-ceramics, and zirconia frameworks have expanded options for full-arch restorations, offering lifelike esthetics and durability. These materials mimic natural teeth’s translucency, color, and texture while providing strength and fracture resistance. They also reduce abrasive effects on opposing teeth, preserving both the artificial and natural dentition. Selecting the right material involves evaluating the patient’s oral environment, bone quality, soft tissue health, bite dynamics, and preferences. Careful assessment and customization improve long-term function and patient satisfaction by creating restorations that blend naturally and are easy to clean, comfortable, and stable against stress.
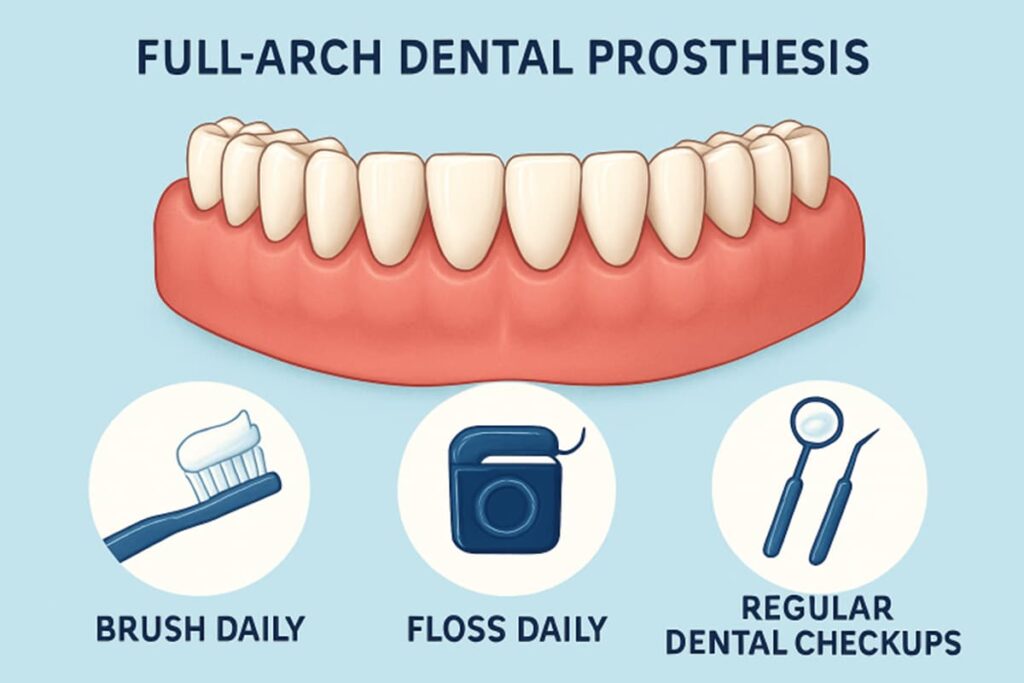
Oral Hygiene and Maintenance
Maintaining excellent oral hygiene is vital for the longevity of full-arch implant prostheses. While these restorations resist decay, soft tissues and bone remain vulnerable to disease if not cared for. Regular professional cleanings every three to six months remove plaque, tartar, and microbes that brushing and flossing might miss. Daily care with interproximal brushes, water flossers, and mouth rinses helps prevent complications like peri-implant mucositis and peri-implantitis, which can lead to bone loss and prosthesis failure. Although these restorations have high survival rates 90% to 98% over 10-15 years the risk of issues rises without regular maintenance. Patients should follow hygiene routines, watch for signs of inflammation or instability, and seek prompt dental help if needed. Routine checkups are crucial for cleaning, exam, and reassessment of fit, ensuring early detection of problems and protecting their oral investment for long-term success.
Occlusal Considerations
Achieving and maintaining a balanced, functional bite is essential to prevent wear or failure of full-arch restorations. Occlusion refers to the way upper and lower teeth or prosthetics come together, and slight imbalances can cause stress to implants or prosthetic parts. Without proper occlusal management, patients risk fractures, screw loosening, component failure, or implant overload, leading to bone loss. Modern dental tools, such as T-Scan and digital analysis, accurately detect minor bite issues.
Identifying and managing parafunctional habits, such as bruxism and clenching, is also crucial, as they exert force on restorations and implants. Patients at risk may be fitted with nightguards or splints to protect their restorations and extend their lifespan. Tailored occlusal schemes help ensure stability, reduce the need for repairs, and promote comfort and longevity.
Dentist Expertise and Techniques
The skill, judgment, and ongoing education of the dental provider are among the most significant factors influencing the outcomes of full-arch restorations. Experienced clinicians tailor therapies, select optimal materials and techniques, and adapt to unforeseen challenges. Emerging technologies like digital impressions, CAD/CAM, and laser-assisted placement improve accuracy, reduce discomfort, and shorten healing. Troubleshooting complications and collaborating with dental technicians ensures precision from template creation to final prosthesis. Continued professional development and staying updated on advances enhance care, satisfaction, and durability. Choosing an experienced team is key to success.
Technological Advancements
Recent technological breakthroughs have greatly enhanced full-arch implant dentistry by improving workflow, accuracy, and predictability. Digital tools like intraoral scanning, 3D imaging, virtual planning, and 3D printing allow high customization in the surgical and prosthetic phases. These technologies enable visualization of anatomy, assessment of bone quality, prediction of complications, and collaboration with specialists and labs. This results in more precise treatment, better-fitting, natural-looking, and comfortable prostheses. Computer-aided manufacturing ensures accurate fabrication, reducing the need for adjustments and improving the long-term fit and function. Virtual planning enhances predictability and can reduce chair time through efficient workflows. As technology advances, patients will experience even greater accuracy, a wider range of material options, and minimally invasive techniques that reduce recovery time and increase overall comfort. Ongoing research and digital integration will broaden access to full-arch implant restorations.
Conclusion
The longevity and functional success of full-arch restorations arise from a dynamic interplay between systemic health, material selection, meticulous hygiene regimes, the expertise of dedicated dental professionals, and the transformative power of digital technology. By taking a comprehensive, individualized approach and fostering open and ongoing communication between patients and providers the pathway to a predictable, confident, and lasting smile remains well within reach for those who embark on this life-changing journey.
Also Read-
- Staying Ahead in Dental Practice: Continuous Education, Tech Trends, and Patient Care
- The Rise of Sleep Health Technology
- Comprehensive Plumbing Care Made Simple